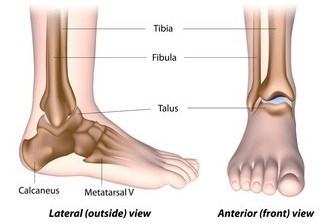
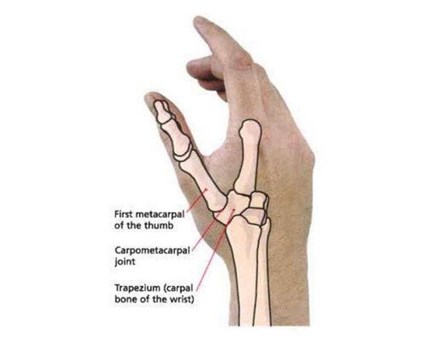
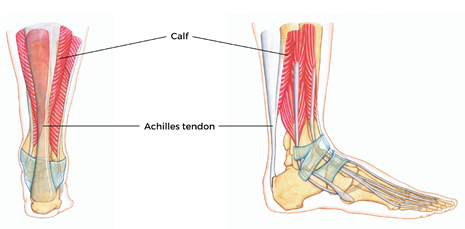
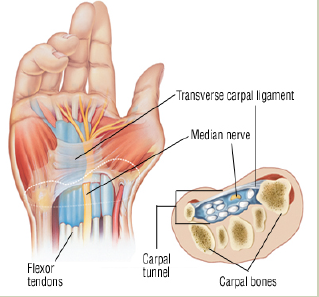
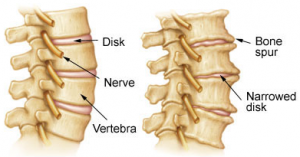
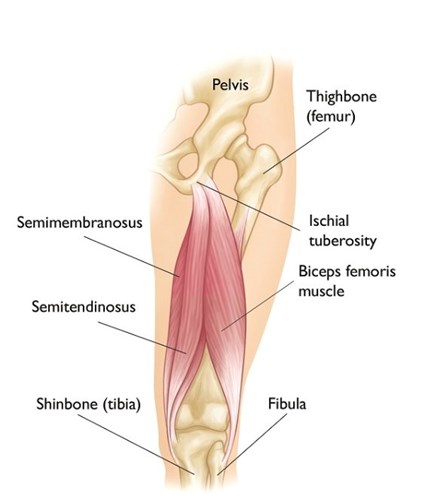
The Achilles tendon is found just behind and above your heel. It joins your heel bone (calcaneum) to your calf muscles. The function of the Achilles tendon is to help you go up on your tip toes, therefore it is involved in walking, running and jumping.
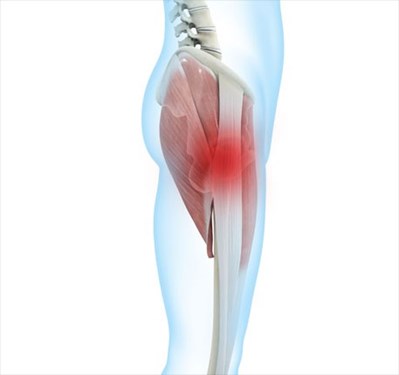
Achilles tendinopathy occurs when the tendon is unable to adapt to the strain being placed on it. This leads to repeated small amounts of damage within the tendon fibres & results in the tendon trying to heal itself in response to the strain. It can occur at the attachment to the heel and in the middle of the tendon.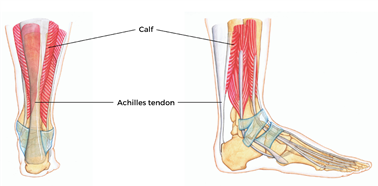
How is it caused?
- Not being fit enough to cope with demands placed on the tendon
- Sudden changes in the intensity or amount of exercise e.g. running
- Repetitive activities
- Tight and/or weak calf muscles
- Stiff joints in the foot
- Smoking and some metabolic conditions e.g. diabetes, high cholesterol raise the risk of having tendon problems
What are the symptoms?
- Pain above the back of the heel, as well as stiffness (especially in the morning)
- Pain after running & while running, which worsens a few hours after the run
- As the pain progresses you find you are unable to run as far before it comes on, and the pain may stick around for an hour or two after exercise.
- It often eases somewhat with activity and exercise
- Tight and stiff calves
- Usually there will be localised swelling at the painful site, forming a bump.
How is it diagnosed?
Diagnosis is generally made clinically following a history taking and physical examination.
What can I do?
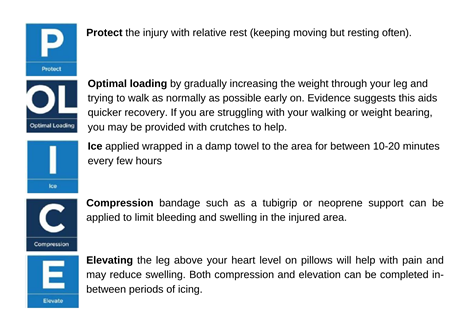
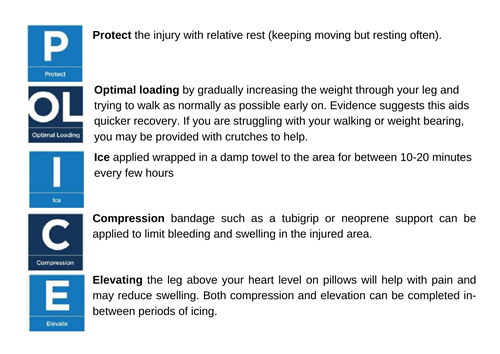
Reduce the tendon’s use:
Reduce the amount of walking and running that you do. Use heel wedges or shoes with a raised heel, including running shoes.
Medication:
Medication such as paracetamol or anti inflammatories such as ibuprofen may also help to reduce your symptoms. If you require further information on pain relief, speak to your GP or pharmacist.
Ice:
Ice the painful site for a maximum of 20 minutes following activity.
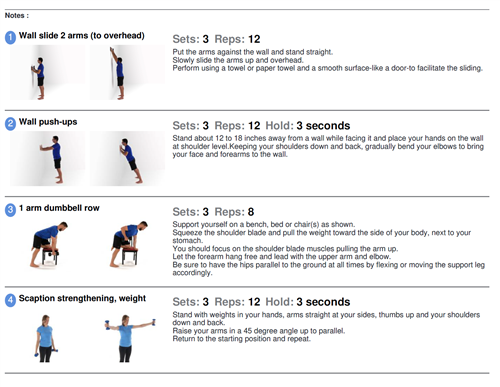
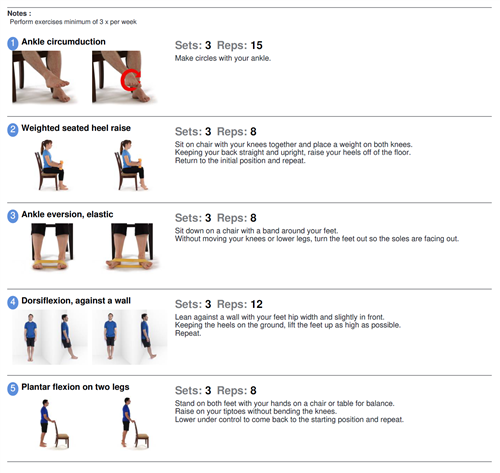
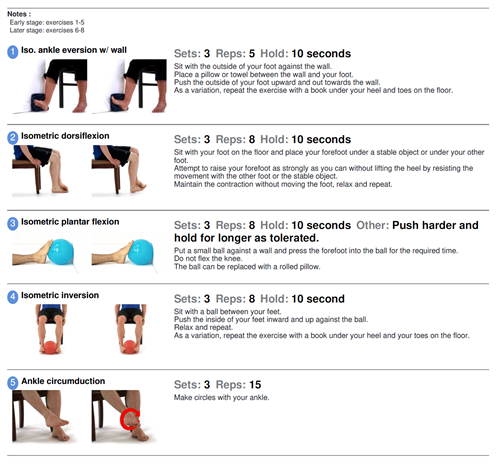
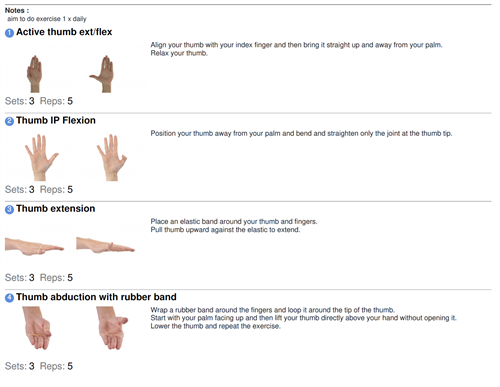
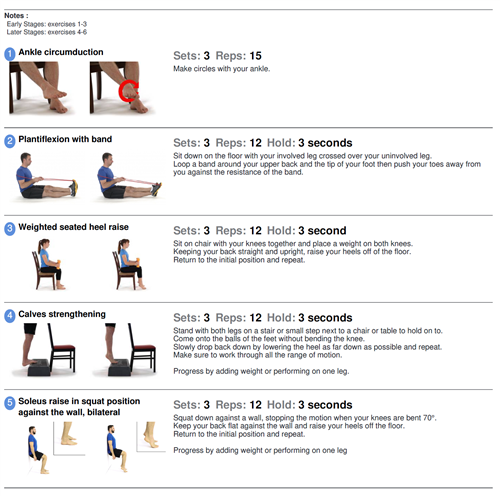
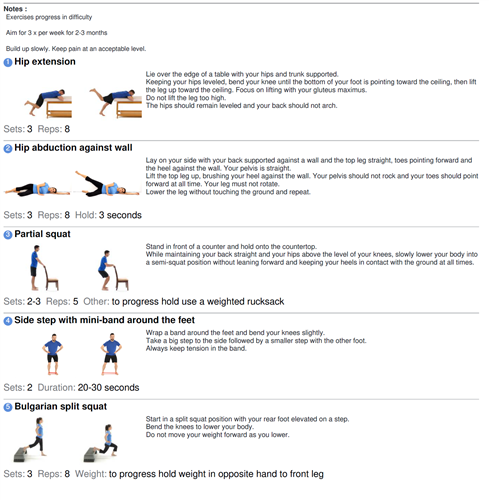
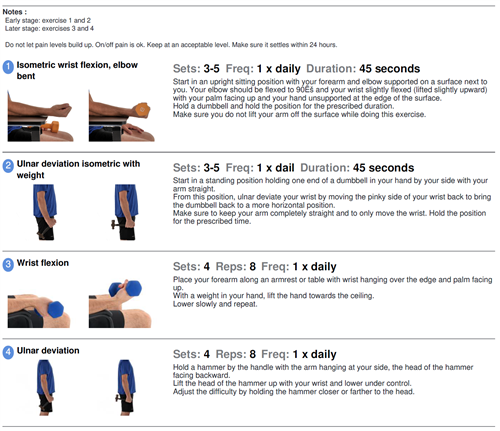
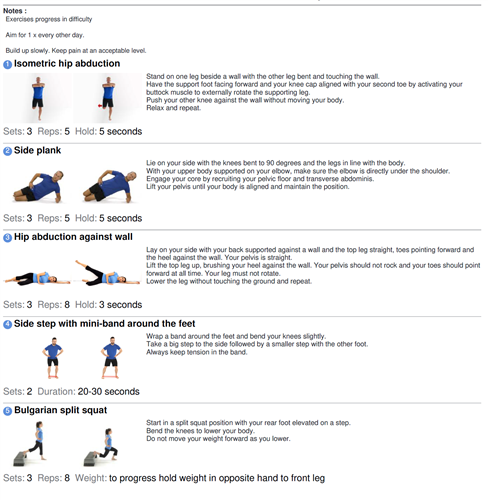
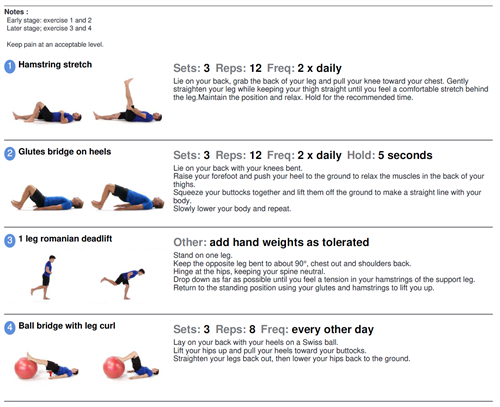
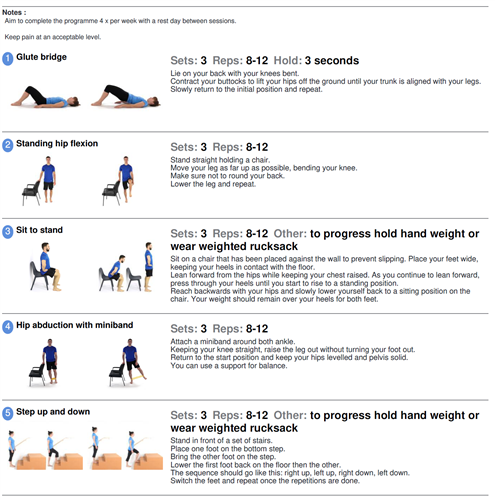
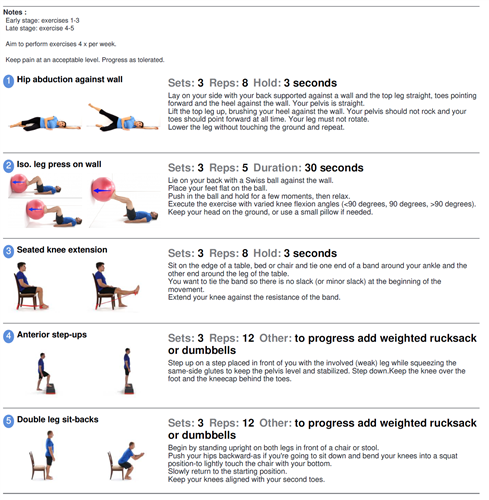
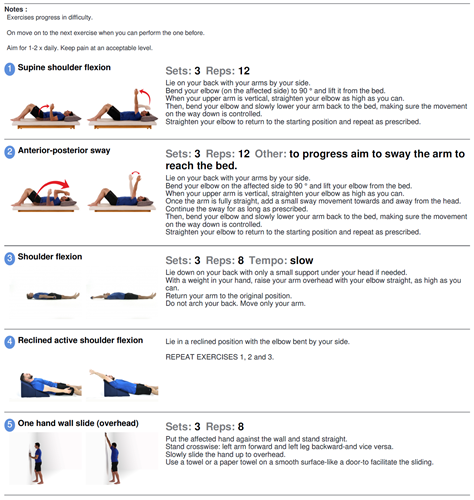
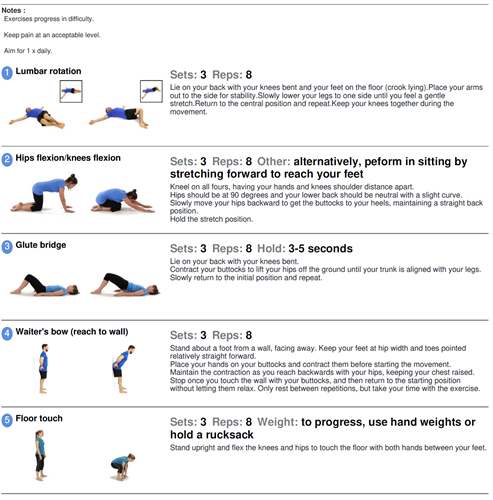
Exercise
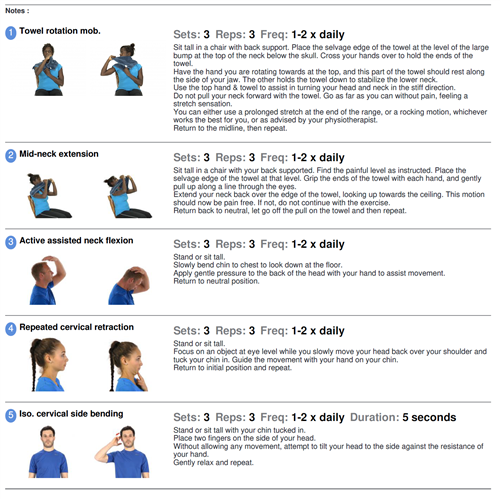
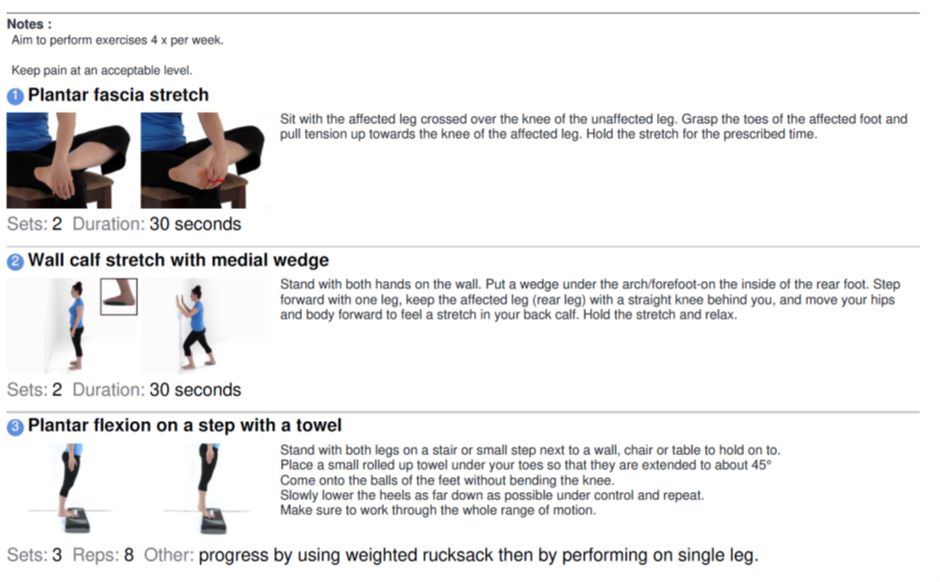
Exercise is an essential towards improving Achilles tendinopathy. Exercises should be done as pain allows, with some discomfort being acceptable as long as it settles within 30 minutes and is not worse the next day. If a sharp shooting pain is provoked then ease off. As your pain reduces and your movement improves consider progressing to the more difficult exercises.
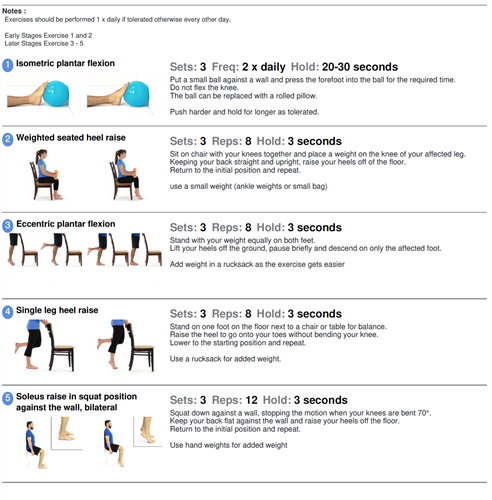
Final stage of recovery
- Continue swimming and cycling as much as the pain will allow.
- If you can do 3 sets of 8-15 repetitions of single leg calf raises comfortably, begin short bursts of jumping, skipping or running on the spot.
- Restart running, beginning on grass for 5-10 minutes, and build up your normal training over the next 2-3 months.
Factors influencing pain and recovery
During your recovery a number of other factors can influence your pain levels. Keep the following factors in mind to help move the healing process along:
Sleep
Sleep is very important for your wellbeing. Poor sleep quality, and lack of sleep can make managing pain more difficult. Consistently getting 6-9 hours is recommended. Get help and tips here: https://www.nhs.uk/live-well/sleep-and-tiredness/
Nutrition and weight
Being overweight can increase the physical strain on the body and also contribute to inflammation in your body. Make sure you eat a balanced diet. Adult weight management services are available free to Essex residents here: https://acelifestyle.org/weight-management
Smoking
Smoking can also impact how quickly tissues can heal and affect pain levels. For help with stopping smoking https://www.essexlifestyleservice.org.uk/stop-smoking/ https://www.nhs.uk/better-health/quit-smoking/
Physical Activity
Maintain your leg, arm and trunk strength whilst also working on specific Achilles exercises. E.g. cycling, body weight exercises or weight training like squats and lunges
Work
You may be worried about continuing with work, or other responsibilities. It is important to discuss these fears with your practitioner. Remaining at work usually leads to a quicker recovery even if you have to work with modified activities.
Your relationship with your boss and colleagues, job enjoyment, feeling supported at work and returning to work are all very important in helping your recovery. Speak to your employer if you need support at work.
Look after yourself
Pain is not usually simply a physical problem. Your general well-being can make you vulnerable to pain and your wellbeing can also be made worse by pain. Looking after your general health and well-being will help recovery. There is helpful advice on this website: https://www.nhs.uk/oneyou
Reduce stress and anxiety
It is normal for people with pain to have stress, anxiety and change in mood. This may affect your ability to cope with the pain and may influence your pain levels. Help is available if you are being affected by stress, anxiety or low mood – see the links below or discuss with your practitioner.
It is important that your whole nervous system is in a healthy state to aid recovery. If your brain is stressed or overworked this may slow recovery. Relaxation is an important part of your recovery. Simple relaxation techniques may help manage pain and stress. Try to set aside some time each day to relax – you can use relaxation techniques as linked below, or simply an activity you enjoy – reading, deep breathing, sitting in the garden, singing – whatever relaxes you.
Find help and support here: https://www.nhs.uk/oneyou/every-mind-matters/
https://www.northessexiapt.nhs.uk/west-essex
How long will it last?
- For most people Achilles tendinopathy can take from 3-6 months to settle down.
- It is important to modify activity until the symptoms settle down while carrying out the exercises
- If there is no improvement in symptoms after following the above advice for 3 months seek help from a Physiotherapist/GP.
What other options are there?
Physiotherapy:
Physiotherapists can provide specialist education and advice regarding exercise. If you wish to receive 1:1 physiotherapy treatment please fill out a self-referral form and send to epunft.mskphysio@nhs.net
Extra corporeal Shockwave therapy
ESWT is a procedure where audible, low energy sound waves are passed through the skin to the injured area. It is a safe minimally invasive treatment but can give some discomfort/pain. It is still uncertain how effective this treatment is for Achilles tendinopathy.
Surgery
This is not routinely recommended and is only considered if symptoms remain disruptive despite the treatments discussed in this leaflet. Surgery generally involves removing the diseased areas of tendon.
Steroid injections are not recommended in or around the Achilles tendon due to the risk of rupture.
Useful websites:
Note: This information is intended as general information only.